Human Health
Making Healthcare a 24/7 Affair
Let’s start with a statement most Americans would agree on: We are all hoping to see more healthcare companies that improve patient outcomes, reduce costs, and increase access to quality care.
Here’s another Obvious line, at least to us: The most valuable healthcare companies of our time will be dramatically elevating outcomes, lowering expenses, and making care more accessible.
Tailwinds from COVID-19 have brightly highlighted latent patient needs while driving meaningful behavioral shifts, unfolding over the course of just a few months with what otherwise may have taken over ten years. In healthcare specifically this is driving extraordinary startup activity, and for us it is a much-needed acceleration of what we’ve believed about outcomes, costs, and accessibility for years: we can leverage a combination of technology and radical empathy to deliver against all three.
We’re keenly aware of the sizable disparities that exist between populations in the U.S., with high risk and rising risk patients having fewer resources at their disposal. As investors, we’re encouraged to see more companies targeting high risk and rising risk individuals with values-based care built on new business models. We’re also beginning to see real results from interventions further upstream, ones creating greater leverage and more efficiencies for healthcare businesses while alleviating stress on our healthcare system overall.
What’s accelerating this the most is not only powerful technology-driven products and services, but the deployment thereof in continuous settings, 24/7.
We believe this anytime, anywhere approach to product and platform development that “meets patients where they are” 24/7 is the best way forward for individuals and our healthcare system overall. It can address the needs of patients across the spectrum (especially those with the most acute), while addressing chronic challenges in ways that save patients’ health, time, and money. The opportunities for entrepreneurs to build these kinds of transformative companies is only growing. Here are three areas of opportunity that get us excited.
I. Segmented
You can’t improve what you don’t measure, and the good news is that we have more tools than ever to help us measure more than before, especially outside the doctor’s office. We are now able to interpret data and make tangible, actionable recommendations based thereupon — and do so with specific populations.
With companies like Devoted Health and Galileo, there are an increasing number of interventions we can take at home. This is critical for Medicare and Medicaid patients, especially those with high and risking risk factors, and at a time when nursing homes are challenged and aging-in-place more appealing on a host of levels. For providers, the technology is helping with triage. And for payors, anything that identifies and mitigates problems upstream will save on costs long term.
The more data we can access (responsibly, of course) and make actionable, the better off all players in the ecosystem will be.
II. Verticalized
Over the past decade, providers have been delivering more effective treatments thanks to not only to the segmentation mentioned above, but also disease-specific approaches driven by breakthrough treatments.
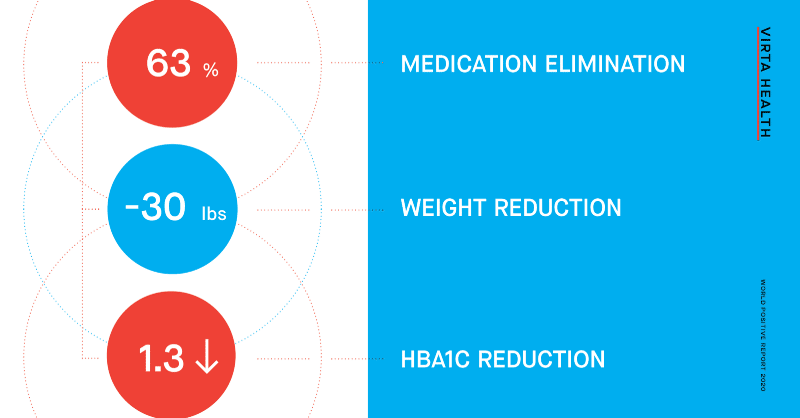
A standout example here is Virta Health, which is using a clinically-validated program to reverse type 2 diabetes (and what’s more, proving that their program can prevent progression from pre-diabetes, and help with weight loss as well).
Another is Octave, an offline/online modern practice supporting all aspects of emotional well-being through therapy — at one quarter the cost of traditional therapy. The results speak for themselves — within twelve weeks, Octave’s therapy clients are seeing:

We’re excited to see this applied across other critical — and massive — categories. Musculoskeletal therapy, long confined to the clinic, is starting to emerge as a home-based category with players like Vori Health. Kidney care, another category dominated by limited players outside the home, is finding its way with companies like Somatus. Seeking access to effective opioid addiction programs is a challenge for millions, with emergent players like Eleanor Health providing ways to increase that accessibility no matter a patient’s location. And with autism, outfits like Positive Development are meeting families where they are by creating more holistic approaches that combine Occupational Therapy, Speech Therapy, and Mental Health Therapy as part of the intervention process.
We see big opportunities especially with companies deploying risk-based models here. And with clinically-validated approaches, all players can align on outcomes — and everyone wins.
III. Ecosystem Platform Enablers
In order to realize the promise of the two categories above, we need more platform players that reduce friction and help meet patients where they are. These ecosystem platform enablers generally sit across three categories: (1) remote patient monitoring (RPM), (2) testing and diagnostics, and (3) logistics.
Advancements in technology have helped us move far beyond the analog days of LifeAlert toward a future with data-centricity, continuous monitoring, and thoughtful triage. More sophisticated approaches are also emerging that bring human-centered healthcare delivery into the home, like Dispatch Health, Medarrive, and Duos.
The field of testing and diagnostics has shifted dramatically over the past ten years. Gone are the days where patients are required to head to a lab facility, with new at-home opportunities at both the consumer-level (with companies like Everlywell) and at enterprise scale (with ixlayer).
And lastly in logistics, we are just beginning to see a streamlining of the process to seamlessly get the right products to patients when and where they need it. Contessa is doing this by bringing hospital-level care into the home, while Tomorrow Health is taking the durable medical equipment space into the 21st Century by matching patients with the most optimal supplier for their needs while simplifying the ordering and reimbursement processes.
Today and into the near future we should continue to raise our standards for overall quality of care, and building toward outcome-driven, more accessible 24/7 products and services can help make it happen. Taking social determinants into account in their design is another emergent practice that we’re excited to see. After all, if patients are food insecure or don’t have other basic needs met, we should be asking how we might solve those at home upstream rather than downstream in the emergency room.
“Do the right thing and you’ll make money” has been a philosophy of mine since my days at Patagonia, and I believe this to be true in healthcare more than ever. If you’re building a company setting new standards of care driven by patient outcomes, meeting patients where they are 24/7, we’d love to connect with you. Drop me a line (vishal [at] obvious [dot] com) or find me on Twitter.
Obvious Ideas







